The next annual meeting of the British Elbow and Shoulder Society is set to take place between 19-21 June 2024. This year sees the event return to the ancestral home of BESS, in Scotland for the first time since its first ever Scientific Meeting. Although this time it will take place at the new venue of the P&J Live arena inside The Event Complex Aberdeen (TECA). The group from LEDA Orthopaedics are thrilled to attend.
Who are BESS?
The British Elbow & Shoulder Society (BESS) has the main goal “to promote for the public benefit the development and advancement of science and health care, in the practice of shoulder and elbow surgery by fostering education, research and clinical excellence amongst surgeons and allied health professionals”. Memberships are available to surgeons and allied health professionals (AHPs), as well as trainees in either case. Oversees practitioners may also become members and so the annual scientific meeting is an excellent networking and learning opportunity.
The organisation was officially founded in 1988 in response to the increasing interest around elbow and shoulder surgery in the UK. The original members Ian Bayley; Michael Watson; Steve Copeland; and Angus Wallace met on 28 March 1987 to discuss what was then the ‘British Shoulder Surgery Association’. It’s since this date that yearly meetings of the BESS have been held.
The motto of BESS, ‘excellence through knowledge’, is upheld by no less than five different committees. These are:
- BESS Council and Trustees.
- Finance Committee.
- Research Committee.
- Shoulder & Elbow Steering Committee.
- Education Committee, with the Instruction Course and Elbow Update Sub-Committees below it.
What to expect at this year’s BESS Scientific Meeting
The British Elbow & Shoulder Society Conference 2024 is supported by many industry partners, and LEDA are proud to be a Silver Supporter for the 2nd consecutive year. Our message to the delegates is clear; we are “Elbow Trauma Specialists”. As such, attendees can expect to learn more about our innovative solutions for elbow trauma surgery on our booth, which is no. 7 this year.
The Instructional Course will take place on Wednesday, June 19th. This is intended to focus on neurological disorders and soft tissue conditions around the elbow and shoulder. Included are a series of lectures on nerve entrapments around the elbow, shoulder neuropathy, assessing nerve injuries, rehabilitation following nerve injury and pathology, stiff elbow condition, and calcific tendonitis. The afternoon symposiums focus on ‘partial thickness tears of the anterior supraspinatus tendon’ and ‘partial & full thickness tears of distal biceps & triceps tendons’ respectively. The day then concludes with a series of debates on case studies and a final panel discussion.
The primary event of the meeting will then take place on the Thursday and Friday of that week (20th-21st). The former consists of three paper sessions, scheduled in between a trade exhibition, a range of masterclasses, and some industry workshops. The final day will then feature another two paper sessions, masterclasses on different areas, and guest lectures. Some examples of the topics covered include:
- Fractures of the distal clavicle and AC joint.
- Elbow arthroscopy for stiff elbow.
- Current evidence on tendon repair and nutrition.
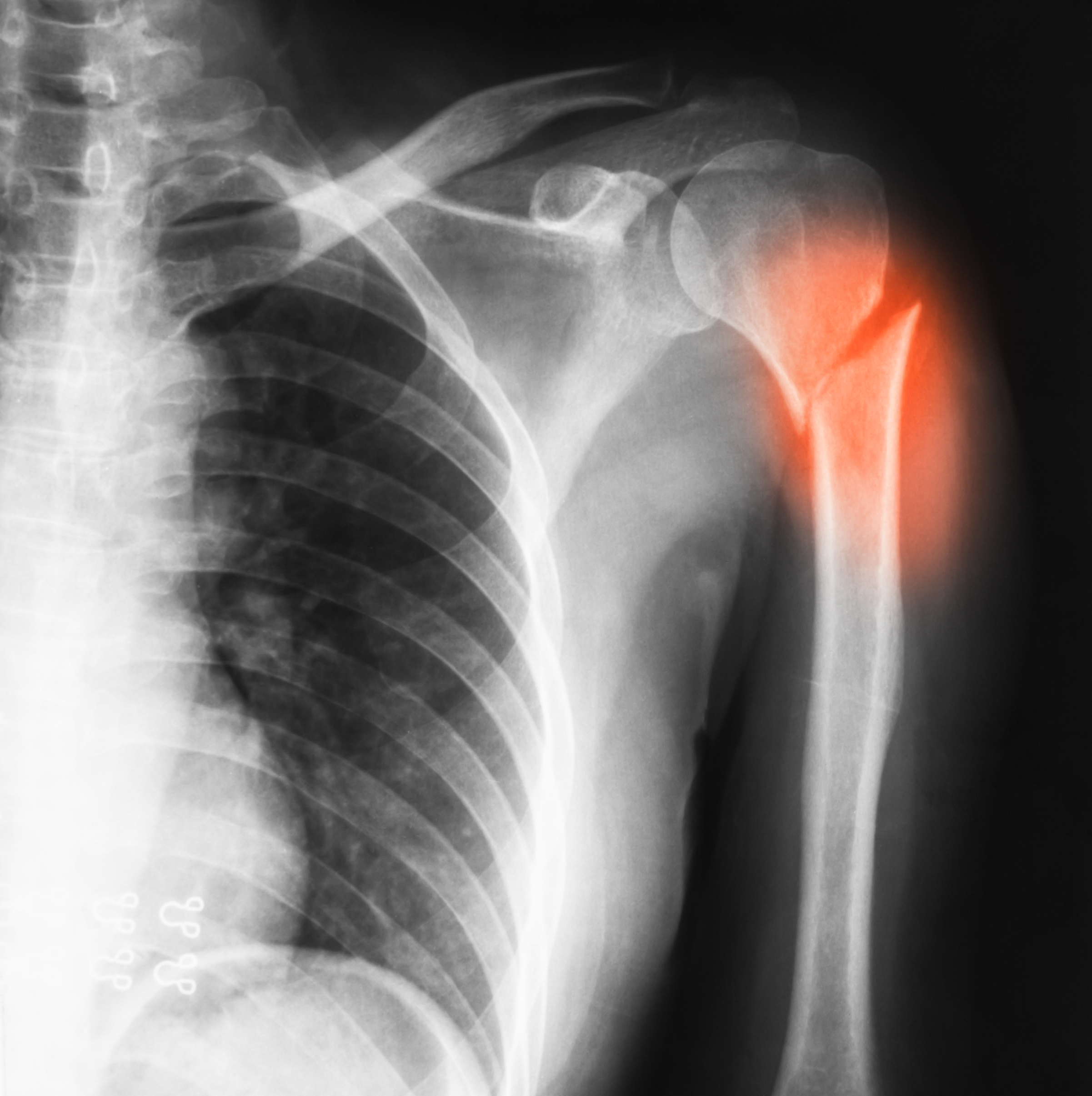
- Proximal humerus fracture.
- Psychological factors associated with shoulder pain.
- Elbow instability.
- Sports injuries of the shoulder.
- Prostheses for radial head replacement.
With our PANTERA – Proximal Humerus Plating system, our Checkpoint Surgical nerve stimulator, and our Jake Design eXo elbow splint, many of the above topics are complimented by the range of products we will be exhibiting.
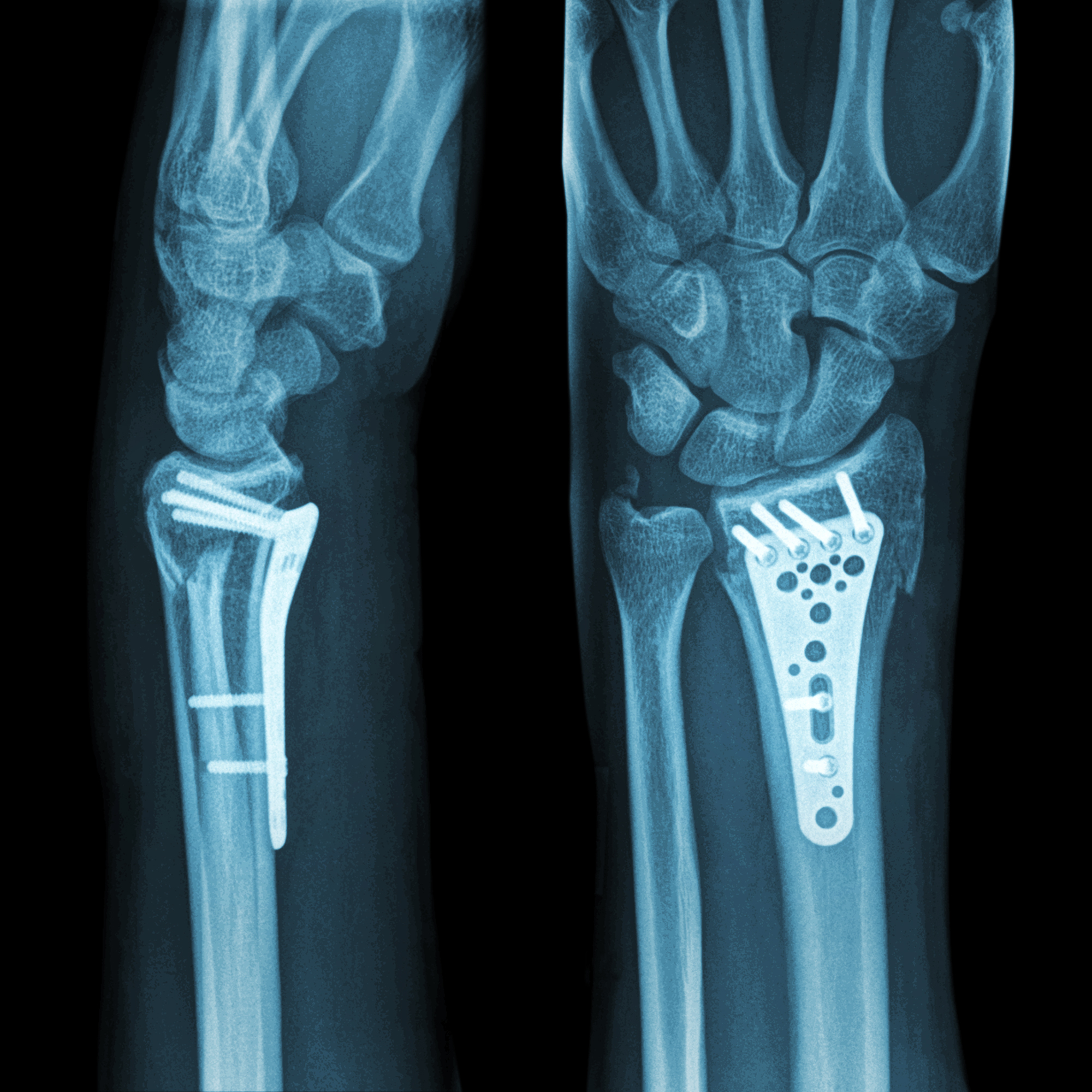
In addition to this, the Skeletal Dynamics’ range of elbow reconstruction systems will allow surgeons to better treat fractures of the elbow using both the Distal Elbow Set and the Humeral Plating System. The game-changing IJS-Elbow always inspires conversations and provides a unique way for surgeons to manage the most complex of elbow cases.
Finally, we will be launching our L3D guides for humeral and glenoid bone preparation for total shoulder replacement, powered by Insight Surgery.
You can find the full provisional programme here.
Looking for a UK medical device distributor?
LEDA Orthopaedics have been providing niche trauma implants, tailored prostheses, and surgical instrumentation for over 10 years. We supply institutions across the NHS and private sector to provide surgeons with the best equipment possible. It’s our belief that orthopaedic innovations are vital to improving patient outcomes following injuries in the upper and lower extremities, especially the elbow and shoulder. Don’t hesitate to contact us if you have any questions, or come find us at the BESS Annual Scientific Meeting 2024.