LEDA Ortho
Established in October 2013, LEDA Orthopaedics began life as a sales agency and quickly grew into a UK and European distributor with innovative suppliers from all over the world. Founding directors David Plane and Jon Bloy have over 30 years’ collective experience in the orthopaedic industry and a passion for the sector that shines through in their commitment to the business to this day. Read More…
We cover the UK and Ireland for:
Latest News

Common causes of proximal humerus fractures
A fracture to the top of the upper arm bone (humerus) can have severe consequences for patients, especially those who are physically active for work or leisure. There can be a number of factors that can contribute to a fracture of the humerus. Being aware of what causes these injuries helps medical professionals deliver better lasting quality of care and improve patient experience. You can find this information further down in the post.
What is a proximal humerus fracture?
Proximal humerus fractures involve the top end of the upper arm bone. This bone runs from the should down to the elbow joint. As a result, it is crucial for many regular arm movements such as opening doors. A proximal humerus fracture can occur in many different forms, with the most common being either a simple or comminuted fracture. Although these fractures can also be classified by the shape or angle of the break, including:
- Transverse fracture.
- Buckle fracture.
- Oblique fracture.
- Segmental fracture.
- Hairline fracture.
- Spiral fracture.
For more detail on how these types of fracture differ, read ‘What’s the difference between a comminuted fracture and a transverse fracture?’.
What commonly causes humerus fracture?
There are a range of factors which can either directly or indirectly contribute to a humerus fracture. Certain causes are more likely to lead to a certain type of fracture, which in turn requires different treatment for proper healing. Knowledge of how a fracture has occurred is useful for planning an osteotomy operation.
Fall
Falling unexpectedly onto an outstretched arm, even from ground level, can result in a humerus fracture. This is a very common cause of upper extremity fracture, as our instinct is always to try and cushion our fall. Older patients or patients that regularly engage in strenuous physical activity are more likely to experience a fall which could risk fracture in the arm.
Accident or injury
An event that causes direct force or pressure to be applied to the shoulder and upper arm can result in a proximal humerus fracture. Examples include car crashes and high-impact sports injuries. The bigger the force, the larger and more complex the fracture is likely to be.
Repetitive stress
Any kind of repetitive motion that places stress on bones can make the individual more susceptible to a fracture. This is because there isn’t adequate time for the body to replace the cells. For humerus fractures, this is commonly caused by weightlifting and sports such as tennis.
Conditions
There are numerous conditions which have the side effect of weakening bones in certain parts of the body. For instance, a metabolic bone disease or bone cysts located around the scapula and upper arm.
Osteoporosis
This condition decreases bone density, resulting in weakness. Individuals with osteoporosis, especially those who have had it for an extended period of time, can suffer a fracture from even a small fall or low-impact trauma event.
Bone tumours
In rare cases, tumours on the bone itself can compromise the strength of the bone and leave it more prone to fracture. It may be necessary to treat the tumours at the same time as the fracture in order to help prevent re-fracture.
Orthopaedic products for fracture fixation
Proximal fractures of the humerus that require internal fixation and reduction must be treated with the appropriate systems. The first step in diagnosing fractures and creating a treatment plan is to investigate the injury site. The L3D Osteotomy Planning and scanning system allows for accurate mapping of internal bone structures. It then analyses the CT scan data to create virtual and physical models for pre-surgical planning. Surgeons can use these models to determine drilling locations and practice cuts ahead of time, serving as specific guides for a patient’s anatomy.
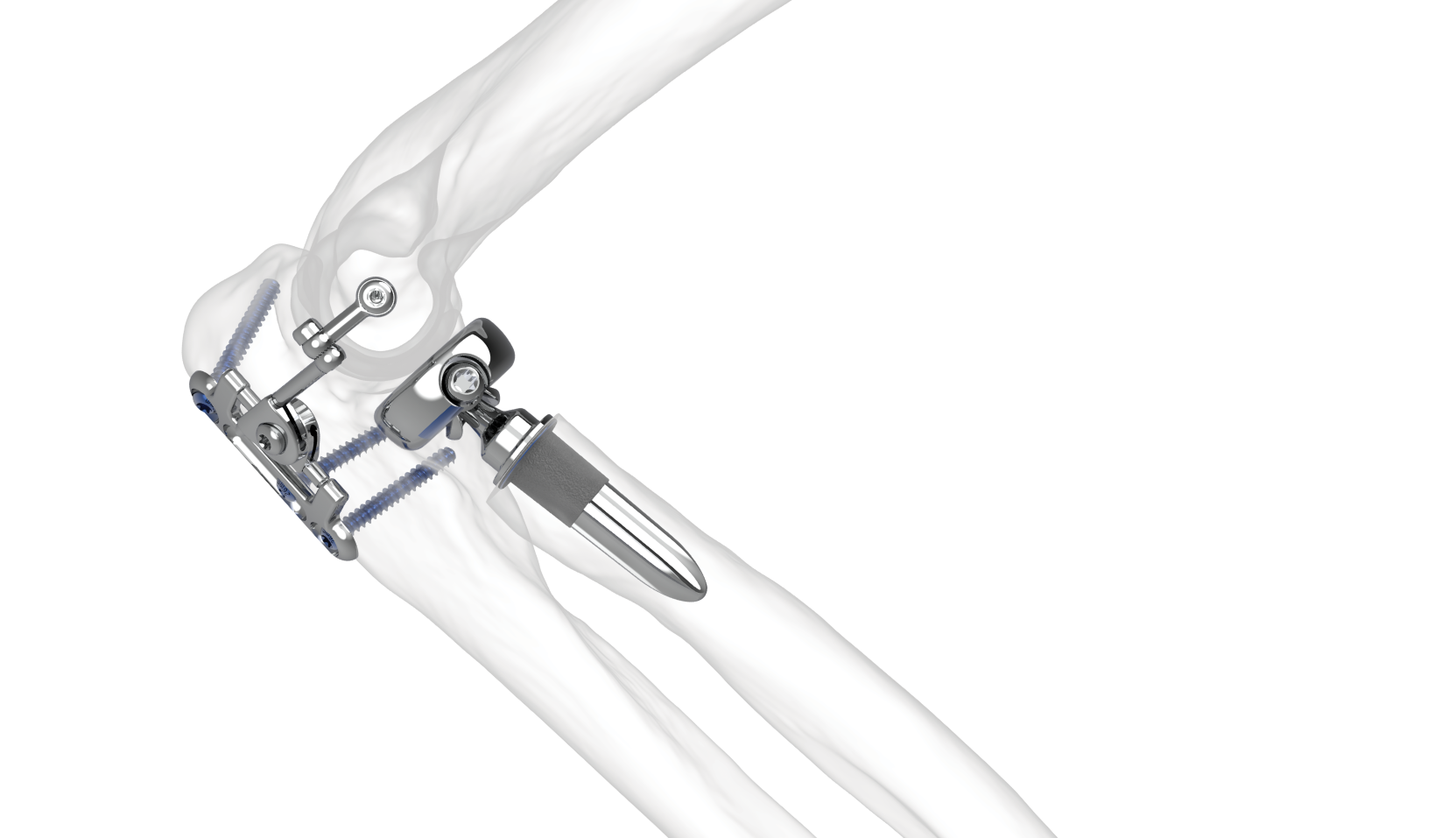
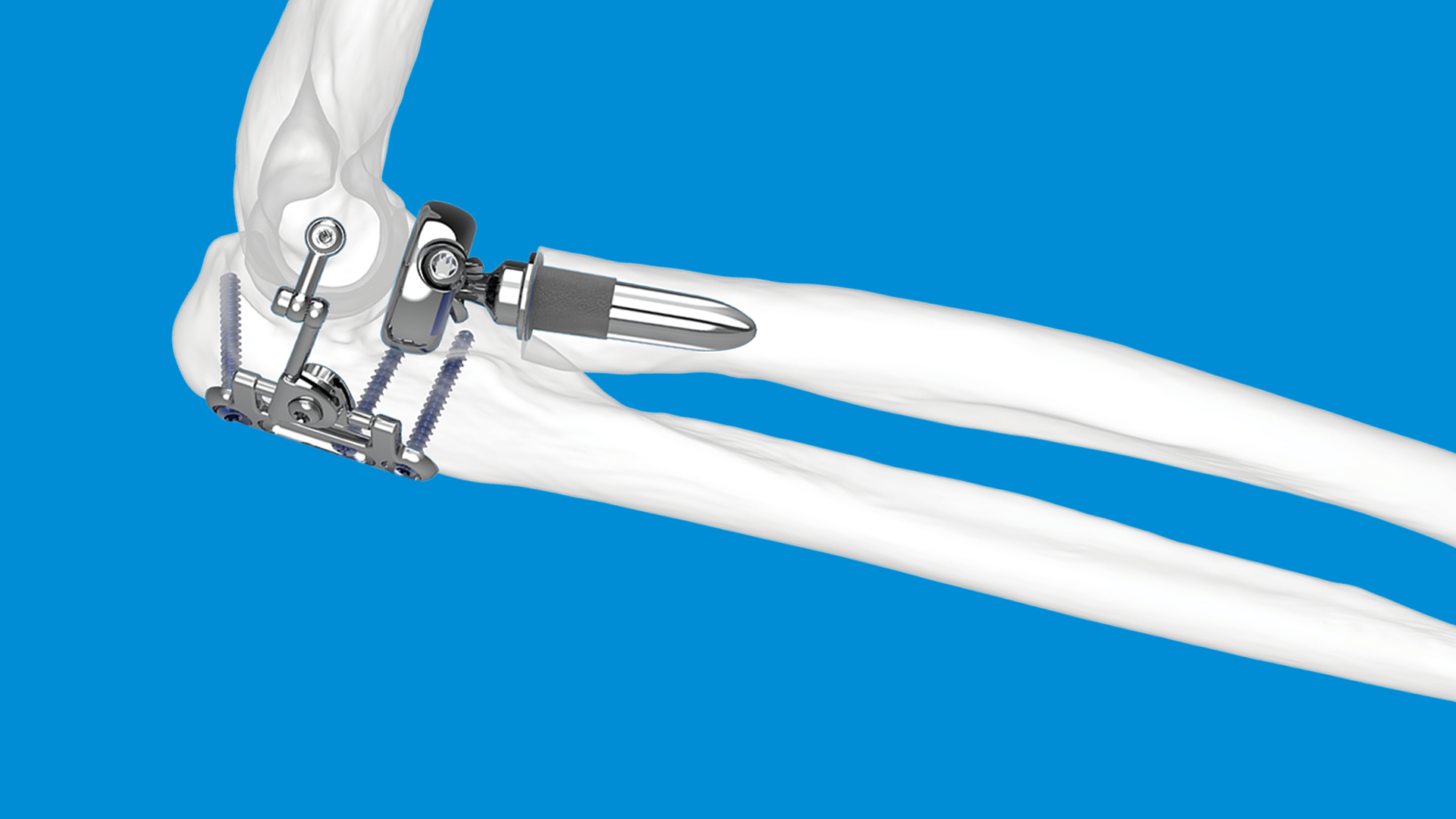
When it comes to fixing the fracture, the PANTERA Proximal Humerus Plate System is a market leading product with advanced options for cross screw fixation and the ability to achieve lesser tuberosity. Proximal humerus plate fixation using this product has been proven to be effective at anatomically reducing and stabilising the humeral head complex. The locking plate design then facilitates regular healing.
Your trusted UK orthopaedic distributor
At LEDA Orthopaedics, we understand the priorities and challenges faced in the medical sector. That’s why we’ve sought to streamline the process of acquiring products for orthopaedic surgeries by including both the system and the relevant instrumentation. This enables practitioners to deliver effective surgical treatment and high quality of care. If you have any questions regarding our elbow & shoulder products, contact LEDA and make an enquiry.




Surgical options for treating a distal radius fracture
Distal radius fractures are among the most common fractures that can affect the hand and wrist. In some cases, non-operative treatments such as arm casting can be prescribed. However, in other cases the best course of action for the patient is for the fracture to be treated with surgery. This post details the surgical options available for treating those with distal radius fractures.
What can cause a fracture in the distal radius?
The most common cause of a distal radius fracture is a fall, as excessive force is placed on the wrist bones at the point of impact. It’s also possible for a fracture to occur in this area due to a sports injury or vehicle collision. The nature of the event that has caused the fracture will determine how complex it is, and at what angle the break occurs.
Surgical treatments for distal radius fractures
Owing to the skill and technology used by modern healthcare professionals, there are a number of different surgical treatments for distal radius fractures. As each can carry different contraindications and potential risks, it’s important that surgeons select the right treatment option for the patient.
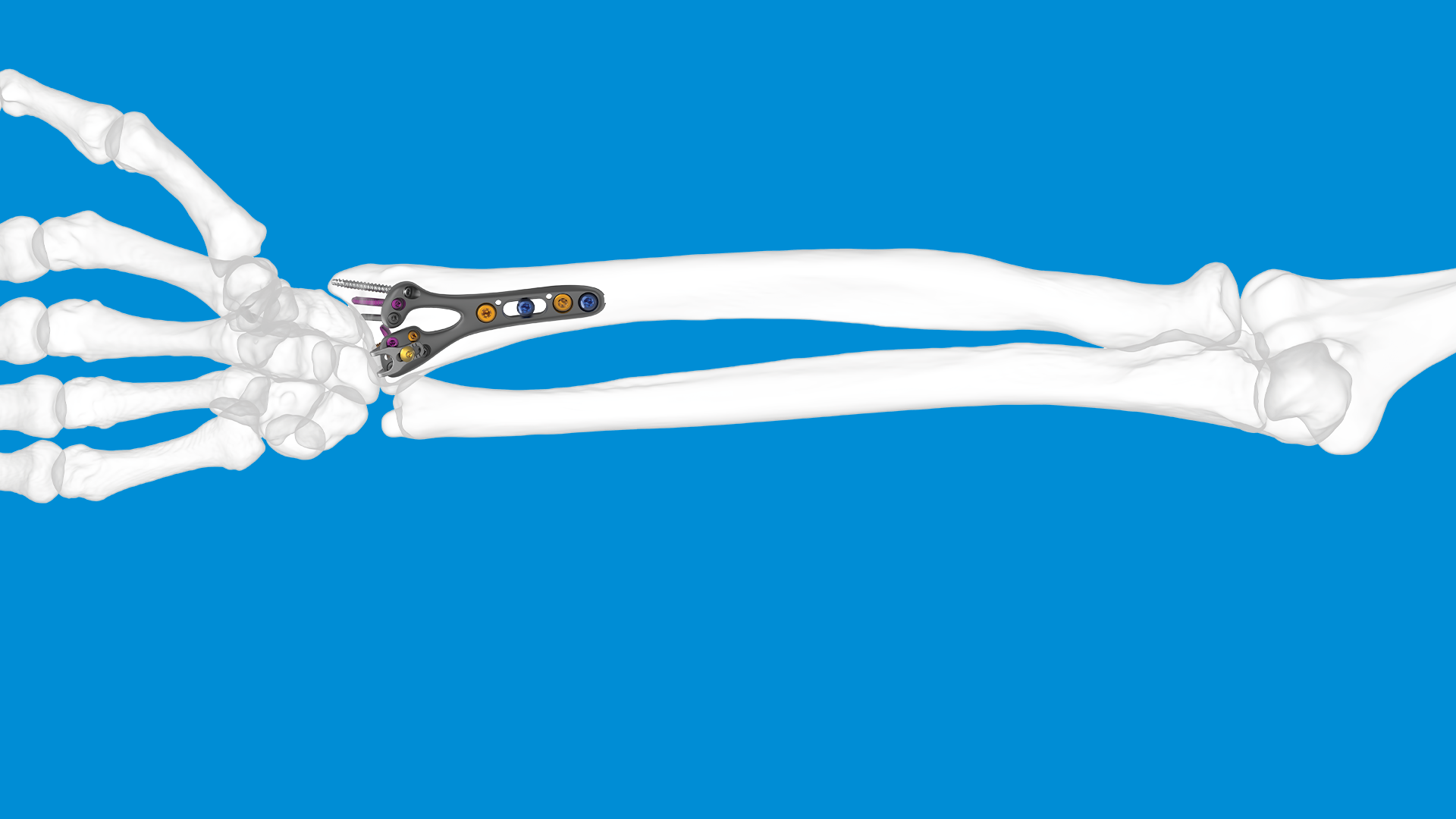
Volar plating
Inserting a purpose-built orthopaedic plate with open reduction and internal fixation (ORIF) is a popular method for fracture treatment. The GEMINUS Distal Radius Volar Plate from Skeletal Dynamics has a contoured design that adheres to a range of patient anatomy. This allows the implant to achieve effective fracture reduction with minimal risk of complications with surrounding soft tissues.
For highly comminuted fractures at the distal radius, surgeons can use the COBRA Distal Radius Hemiarthroplasty prosthesis. This radial implant is intended to restore stability at the fracture site.
Dorsal plating
Surgery to implant dorsal plating follows a largely similar approach to that used for volar plating. However, this treatment is frequently used to treat complex fractures with fragment specific plates. Devices such as that included in the PROTEAN system, follows a modular design to achieve fixation of each individual bone fragment.
External fixation
This procedure involves placing pins into the bone that then extend beyond the surface of the skin. An external frame is then used to stabilise the bone and limit movement for healing. Variations of external fixation can be implemented depending on the patient’s situation. For instance, the frame fixator can extend across the wrist to keep it completely static, or it can feature a hinge to allow basic joint motion.
Orthopaedic solutions for radius fractures
LEDA Orthopaedics is a leading UK distributor supporting surgeons in providing treatment options for fractures of all kinds. We recognise that fractures are among the most common injuries that can be sustained people of all ages, especially in the upper and lower extremities. That’s why we’re partnered with leading orthopaedic suppliers from around the world. Contact us today and we’ll be happy to discuss how the needs of your facility can be met.




Treatments for hand and wrist osteoarthritis
Arthritis is a condition that is likely to affect many of us in our lifetime, especially as we get older. A Versus Arthritis study from 2023 reports that there are roughly 10 million people in the UK living with osteoarthritis, with an estimated 350,000 being diagnosed with the condition each year. Given that osteoarthritis is more problematic when it affects joints that see regular use, let’s examine the treatment options available for osteoarthritis of the hand and wrist.
Defining wrist osteoarthritis
Osteoarthritis in the wrist causes the soft tissue lining the joints to break down. When this happens, the cartilage can no longer serve its protective function and the two ends of bone begin to rub together (distal radius/ulna and scaphoid/lunate/triquetral). The result can be pain and stiffness at the affected area, along with potential loss of movement and bone deformities. Arthritis in any form is also one of the main contributing factors in upper and lower extremity fractures, such as a distal radius fracture. Read ‘Common causes of upper extremity fractures’ for more information.
What’s the difference between arthritis and osteoarthritis?
Osteoarthritis is a degenerative form of arthritis which is caused by wear and tear from excessive use of the affected joints. It is also the most common type of arthritis. While there are many more types of arthritis that can affect the bones in the hand and wrist, the other common types include Rheumatoid arthritis and Psoriatic arthritis.
What areas does hand osteoarthritis commonly affect?
Although osteoarthritis is common in the hand due to the number of different bones, it rarely affects all parts of the hand and wrist equally. Instead, it most often affects the following joints in the hand:
- The distal interphalangeal joint (DIP joint).
- The proximal interphalangeal joint (PIP joint).
- The trapeziometacarpal joint (TMC joint).
- The carpometacarpal joint (CMC joint).
- The tri-scaphoid joint (STT joint).
Treatment options for osteoarthritis of the hand and wrist
At the time of writing, it is still unclear what the root cause of osteoarthritis is. However, medical professionals like LEDA are aware of the factors that can make an individual more susceptible to hand and wrist osteoarthritis. This includes a patient’s age, weight, injuries, hobbies, sex, genetics, and any underlying joint health problems. Fortunately, there are many treatment options both orthopaedic and non-orthopaedic that surgeons may employ in cases of osteoarthritis.
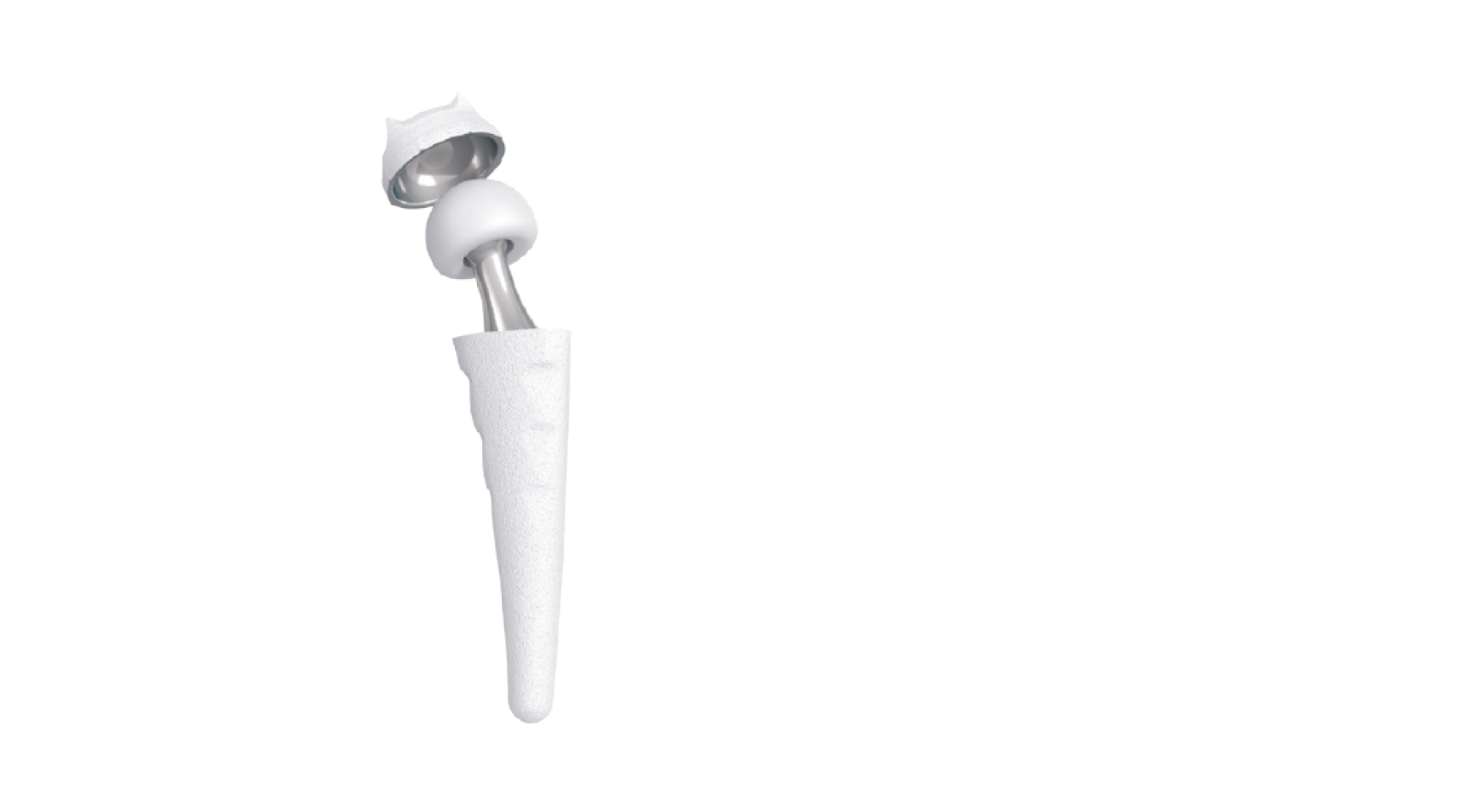
MAIA CMCJ Replacement
One of the key areas in the hand that is susceptible to osteoarthritis are the carpometacarpal and trapeziometacarpal joint at the base of the thumb where it meets the wrist. This orthopaedic device from Group Lépine is a surgical treatment designed to restore motion and provide stability to the thumb. It consisted of a cup, neck, and stem which, when implanted, connect the two ends of bone at the joint. This is an osteotomy procedure as small pieces of bone at the joint must be removed to allow for the implantation of the MAIA device, which serves as a thumb joint replacement.
INCA STT Prosthesis
In cases of scaphotrapeziotrapezoid osteoarthritis, surgeons can use the INCA STT prosthesis for lasting treatment. The implant has been designed anatomically to make sure it fits perfectly with the anatomy of the patient’s joint surfaces. Stability is then encouraged through the stem shape, thereby requiring standard instrumentation to complete the procedure. This device can also achieve cementless fixation due to its double coating of porous titanium.
IMPLATE Wrist Arthrodesis Nails
The IMPLATE system from Skeletal Dynamics is intended for intramedullary wrist arthrodesis to restore strength and dexterity to the hand and wrist. This is an ideal treatment following a range of arthritis symptoms, including rheumatoid deformities, carpal instability, unremitting wrist pain, post septic arthritis, and more. A wrist arthrodesis plate such as this is effective at achieving. While the surgical technique for this implant contains more steps than most other hand and wrist orthopaedic devices, it can be the best option for patient quality of life. As well as osteoarthritis symptoms, IMPLATE can be used to treat trauma injuries (fractures) and congenital deformities.
Physical therapies
If it’s deemed the best course of action, there are a range of non-invasive treatment options for hand and wrist arthritis in the form of hand osteoarthritis exercises. These should focus on gentle movements that improve range of motion and help alleviate arthritis symptoms. Although the exact type of exercises prescribed will vary depending on the joints affected by the condition in that patient.
Orthopaedic devices for the treatment of osteoarthritis
LEDA Orthopaedics is a leading UK orthopaedic distributor committed to helping healthcare professionals deliver great patient outcomes. To this end, we work with suppliers all over the world with a focus on both the upper and lower extremities. One of the key areas these treatments target is osteoarthritis in the hand and wrist, as we know how many people it affects. Contact us to discuss our range of treatment options. Equally, if you are looking for one of our suppliers, we’re always happy to pass details over and establish working relationships.
The Founders